Table of Contents
I. Introduction
Welcome to the second part of our blog series on managing preeclampsia. In the previous article, we discussed what preeclampsia is, its causes, and the signs and symptoms to watch out for. In this installment, we will delve into the management strategies that can help ensure a healthy pregnancy for both the mother and baby. If you or someone you know has been diagnosed with preeclampsia, read on to discover important information and practical tips for managing this condition.
Il. Regular Prenatal Care:
One of the crucial aspects of managing preeclampsia is consistent prenatal care. Regular check-ups with your healthcare provider will enable them to closely monitor your blood pressure, assess your overall health, and detect any potential complications early on. Attend all scheduled appointments and follow your healthcare provider’s advice diligently.
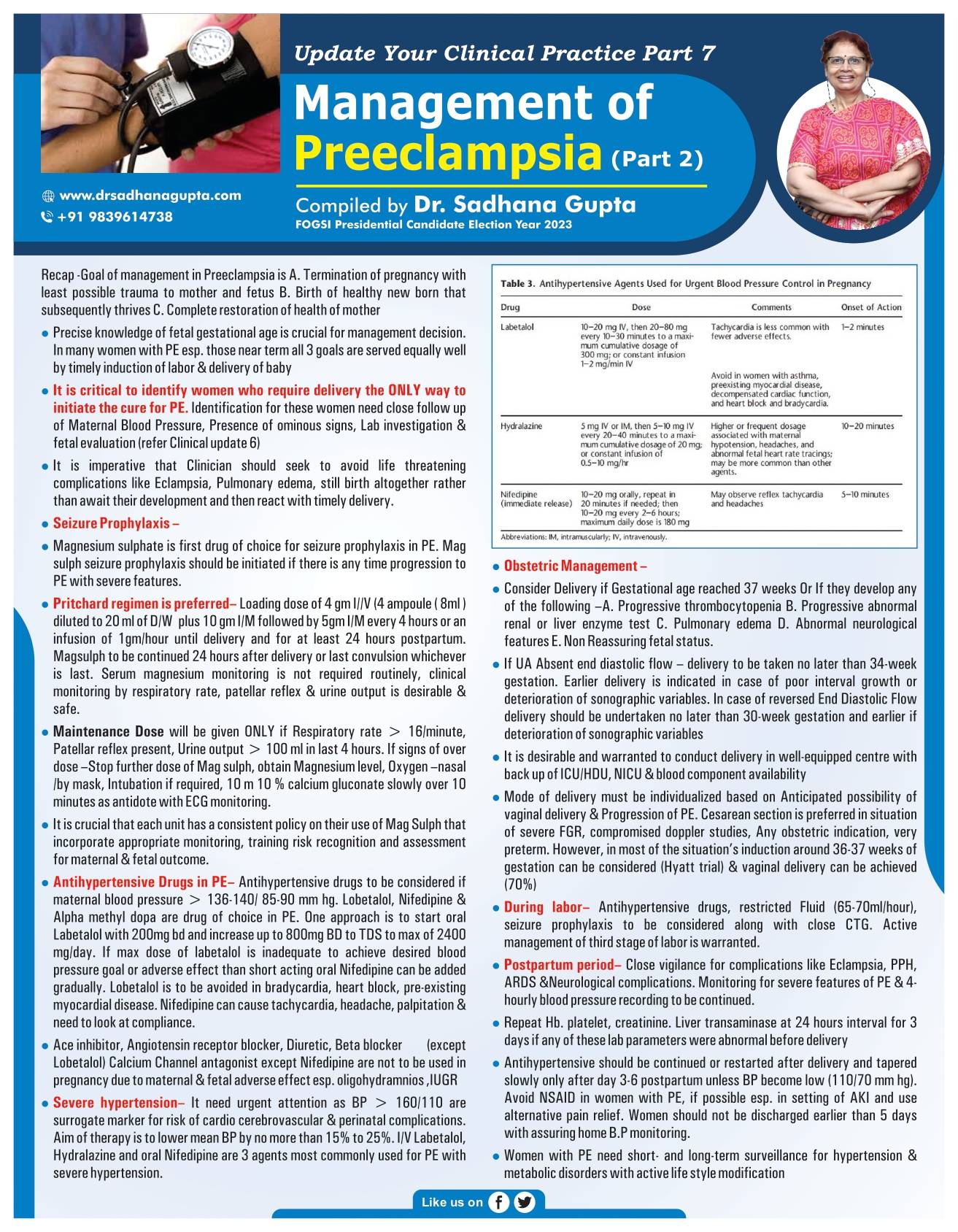
III. Medications:
Your healthcare provider may prescribe certain medications to help manage preeclampsia and its symptoms. These medications might include antihypertensive drugs to control high blood pressure, corticosteroids to promote fetal lung development, and medications to prevent seizures (if necessary). Take all medications as prescribed and inform your healthcare provider of any adverse reactions or concerns.
IV. Bed Rest and Activity Modification:
In some cases, bed rest or reduced physical activity may be recommended to help manage preeclampsia. Resting on your left side can improve blood flow to the placenta and relieve pressure on major blood vessels. However, the extent of bed rest and activity modification will vary depending on the severity of your condition. Follow your healthcare provider’s instructions regarding the level of activity that is safe for you.
V. Dietary Modifications:
Adopting a healthy and balanced diet is essential for managing preeclampsia. Your healthcare provider may recommend a low-sodium diet to help control blood pressure. Include plenty of fruits, vegetables, whole grains, and lean proteins in your meals. Avoid processed foods, excessive salt intake, and foods high in saturated fats. Additionally, it is important to stay hydrated by drinking an adequate amount of water throughout the day.
Monitoring Blood Pressure at Home:
Regular monitoring of your blood pressure at home, in addition to your healthcare provider’s visits, can provide valuable information about your condition’s progression. Your healthcare provider can guide you on how to measure your blood pressure accurately at home and what values to look out for. Keep a record of your readings and share them with your healthcare provider during appointments.
Fetal Monitoring:
Continuous monitoring of your baby’s well-being is crucial in managing preeclampsia. This may involve regular ultrasounds to assess fetal growth, as well as non-stress tests or biophysical profiles to monitor the baby’s heart rate, movements, and amniotic fluid levels. These tests can help determine the appropriate timing of delivery if the condition worsens or becomes severe.
Hospitalization and Delivery:
In severe cases of preeclampsia, hospitalization may be necessary to closely monitor both the mother and baby. Depending on the severity and gestational age, your healthcare provider may recommend inducing labor or performing a cesarean delivery to protect the health and well-being of both you and your baby.
VIII. Conclusion
While preeclampsia can be a challenging condition to manage, with appropriate medical care and lifestyle modifications, you can navigate through it and have a healthy pregnancy. Remember, early detection, regular prenatal care, medication adherence, and close monitoring are key to ensuring the best possible outcome for both you and your baby. In the next part of this series, we will explore postpartum care and the long-term implications of preeclampsia. Stay tuned for more