Table of Contents
I. Introduction
Welcome back to the second part of our blog series on Fetal Growth Restriction (FGR). In the previous article, we discussed the definition, causes, and risk factors associated with FGR. In this installment, we will delve into the important topic of diagnosing FGR. Early detection and accurate diagnosis are crucial for managing FGR and ensuring the best possible outcome for both the mother and the baby. So, let’s explore the various diagnostic methods used for FGR.
Section 1: Ultrasound:
Ultrasound is the primary tool used for diagnosing FGR. It allows healthcare providers to visualize the baby’s growth and monitor key parameters throughout pregnancy. The following ultrasound measurements are commonly used:
a) Abdominal circumference (AC): This measurement assesses the size of the baby’s abdomen, reflecting its overall growth.
b) Head circumference (HC): HC measurement helps evaluate the baby’s brain development and can provide important insights into FGR.
c) Femur length (FL): FL measurement estimates the length of the baby’s femur bone and aids in assessing skeletal growth.
d) Estimated fetal weight (EFW): EFW is calculated by combining the measurements mentioned above. It provides an estimate of the baby’s weight and helps determine if it is consistent with the gestational age.
a) Abdominal circumference (AC): This measurement assesses the size of the baby’s abdomen, reflecting its overall growth.
b) Head circumference (HC): HC measurement helps evaluate the baby’s brain development and can provide important insights into FGR.
c) Femur length (FL): FL measurement estimates the length of the baby’s femur bone and aids in assessing skeletal growth.
d) Estimated fetal weight (EFW): EFW is calculated by combining the measurements mentioned above. It provides an estimate of the baby’s weight and helps determine if it is consistent with the gestational age.
Section 2: Doppler ultrasound:
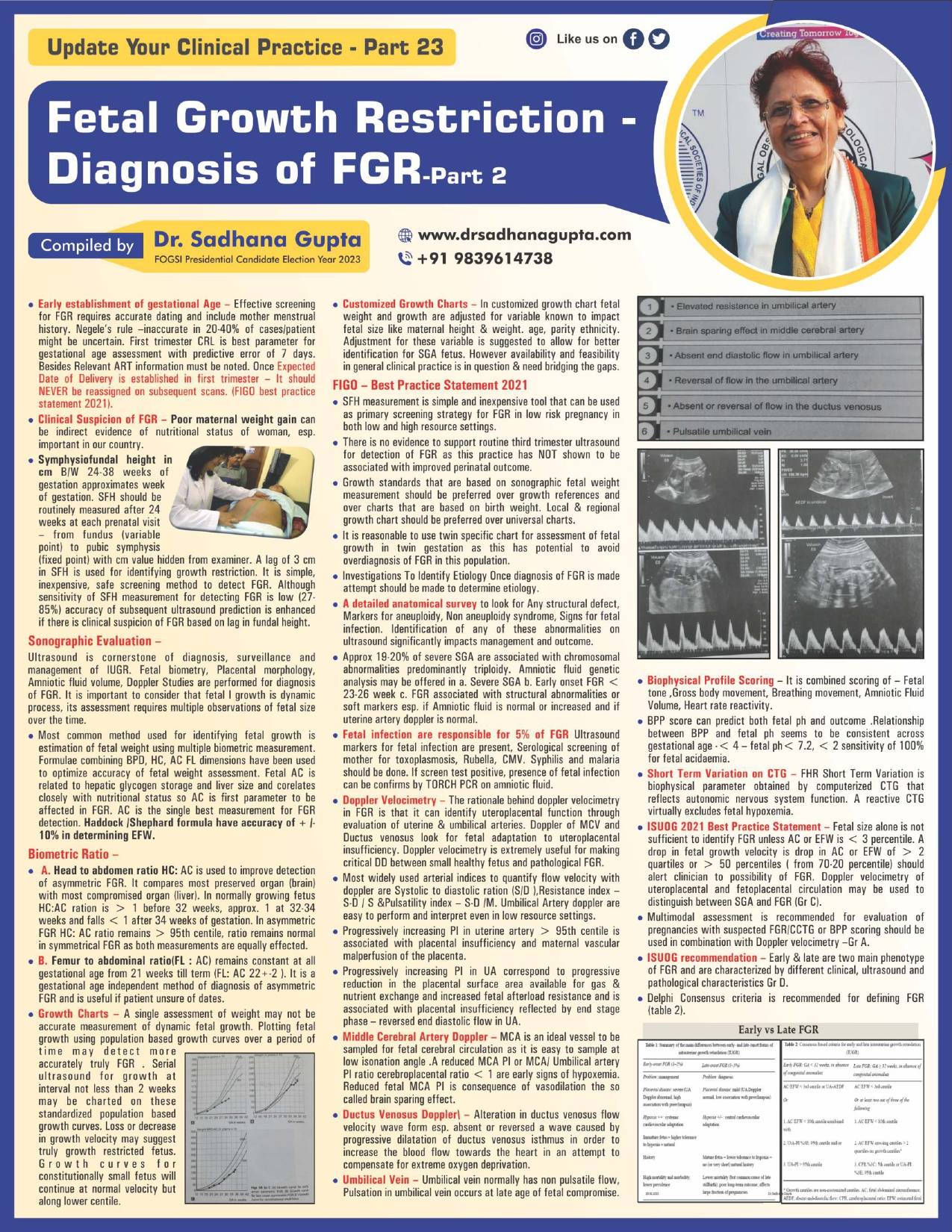
Doppler ultrasound is a specialized type of ultrasound that evaluates blood flow in the baby’s arteries and veins. It plays a crucial role in assessing the placental function and detecting any abnormalities that may contribute to FGR. Doppler studies focus on the umbilical artery, middle cerebral artery, and uterine arteries.
a) Umbilical artery Doppler: This measurement assesses the blood flow in the umbilical artery, which supplies oxygen and nutrients to the baby. Abnormal flow patterns, such as high resistance or absent end-diastolic flow, can indicate problems with placental function.
b) Middle cerebral artery Doppler: This measurement evaluates the blood flow in the baby’s brain. Changes in cerebral blood flow can indicate fetal distress and help diagnose FGR.
c) Uterine artery Doppler: Uterine artery Doppler studies provide information about the mother’s blood flow to the placenta. Abnormal flow patterns may suggest placental insufficiency, which can lead to FGR
a) Umbilical artery Doppler: This measurement assesses the blood flow in the umbilical artery, which supplies oxygen and nutrients to the baby. Abnormal flow patterns, such as high resistance or absent end-diastolic flow, can indicate problems with placental function.
b) Middle cerebral artery Doppler: This measurement evaluates the blood flow in the baby’s brain. Changes in cerebral blood flow can indicate fetal distress and help diagnose FGR.
c) Uterine artery Doppler: Uterine artery Doppler studies provide information about the mother’s blood flow to the placenta. Abnormal flow patterns may suggest placental insufficiency, which can lead to FGR
Section 3: Serial measurements:
Serial measurements involve monitoring the baby’s growth parameters over time. Regular ultrasounds and Doppler studies at specific intervals can help identify any deviations from the expected growth pattern. Serial measurements are especially important in high-risk pregnancies or when FGR is suspected.
Section 4: Maternal assessment:
Apart from ultrasound and Doppler studies, healthcare providers also consider maternal symptoms and risk factors when diagnosing FGR. Maternal factors such as hypertension, preeclampsia, chronic medical conditions, or history of previous FGR can contribute to the diagnosis.
Conclusion:
Diagnosing Fetal Growth Restriction (FGR) requires a comprehensive approach that combines ultrasound measurements, Doppler studies, and maternal assessment. Early detection and accurate diagnosis play a crucial role in managing FGR and minimizing the risks associated with it. If FGR is suspected, close monitoring and appropriate interventions can help optimize outcomes for both the mother and the baby. In the next part of our series, we will discuss the management and treatment options for FGR. Stay tuned!